Conventional in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI) are two of the most widely used techniques in assisted reproduction treatments.
Both share the same objective: to obtain viable embryos in the laboratory and then transfer them to the woman's uterus.
However, they differ in the strategy to achieve this goal.
What is the difference between conventional IVF and ICSI?
The main difference between the two techniques lies in the way in which oocyte fertilisation occurs.
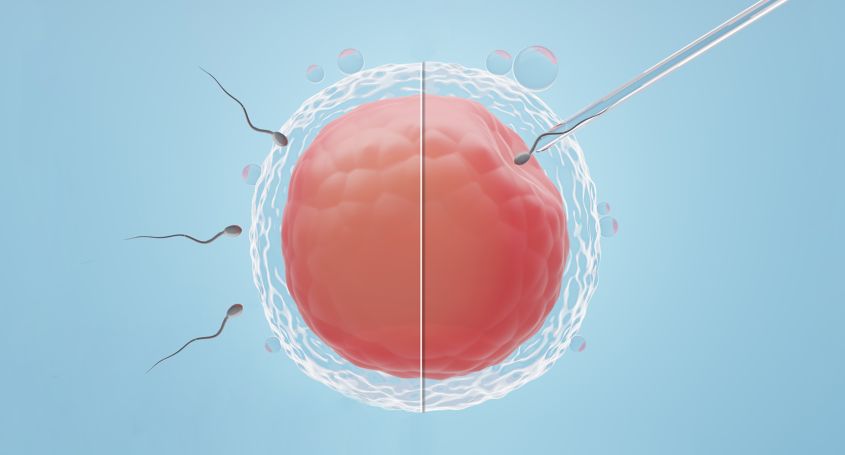
In conventional IVF, the sperm are placed together with the eggs in a culture medium, simulating the natural mechanism of fertilisation. In this way, the sperm must reach and penetrate the egg, mimicking the natural fertilisation process.
In ICSI, on the other hand, the embryologist selects a single sperm and microinjects it directly into the cytoplasm of the egg.
What are the advantages and disadvantages of each technique?
The main attraction of conventional IVF is that it reproduces, in a controlled manner, the natural process of fertilisation. It allows spermatozoa to compete with each other to penetrate the egg, favouring the fittest and reducing the direct manipulation of the gametes.
Its main limitation is the risk that the oocytes will not be fertilised.
ICSI, on the other hand, maximises fertilisation even with semen samples of poor quality or quantity, or when the number of oocytes retrieved is limited. By giving the embryologist full control of the process, fertilisation failures are significantly reduced. Its main disadvantage is that it requires more manipulation of the gametes.
When is each technique chosen?
The decision to use conventional IVF or ICSI is made by the medical team together with the embryologist after evaluating each case individually. This assessment takes into account the quality of the sperm, the quantity and quality of the eggs and the couple's reproductive history.
In general, conventional IVF is usually appropriate in cases of infertility not related to gamete quality or quantity, such as tubal blockages.
ICSI, due to its higher reliability, is recommended when there is a significant male factor, when the number of oocytes or sperm is low, when frozen semen samples are used, or in procedures requiring pre-implantation diagnosis.
In clinical practice, there is no "best" technique in absolute terms. What is really important is to choose the most appropriate option for each case, according to its specific characteristics and needs.
However, in daily practice, most centres routinely use ICSI to maximise results and to avoid cases of fertilisation failure using conventional IVF.
At Barcelona IVF we take care of the whole process, from the choice of the most suitable fertilisation technique to the optimisation of all the factors of the cycle: ovarian stimulation, embryo quality and transfer.
Dr. Cristina Guix
Fertility expert gynaecologist in Barcelona IVF