Male sterility represents almost 50% of infertility problems. When we face several pathologic semen analyses or when pregnancy is not achieved despite having normal semen analyses, a complete andrological examination is recommended.

Male sterility represents almost 50% of infertility problems. When we face several pathologic semen analyses or when pregnancy is not achieved despite having normal semen analyses, a complete andrological examination is recommended.
Examination of male sterility includes the following diagnostic tests
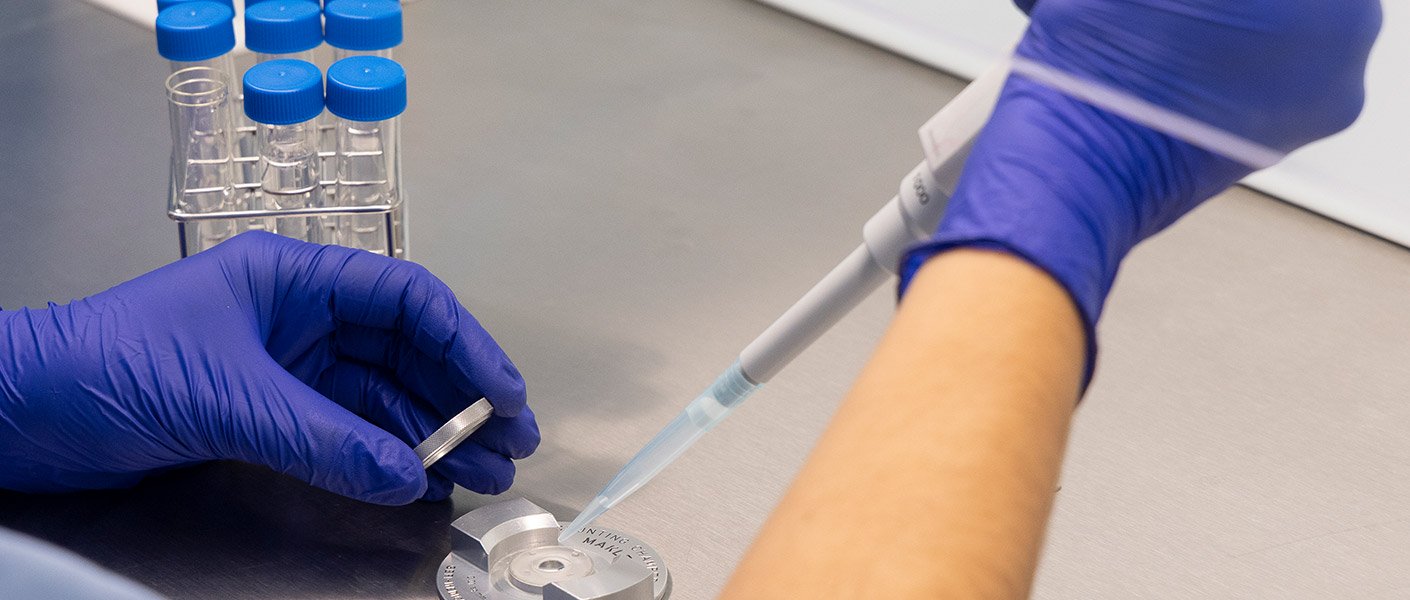
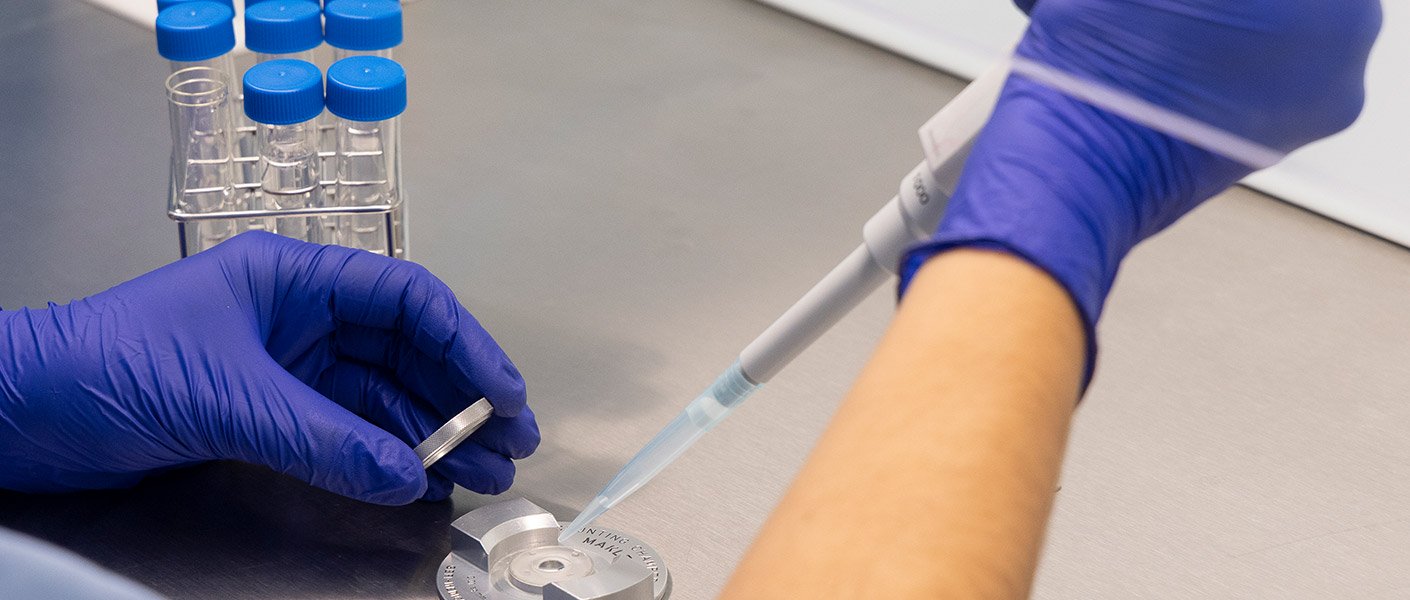
A semen analysis informs us about the sperm count, motility and morphology.
In order to interpret the results of a semen analysis, we need to apply the normal values established by the WHO in 2009:
There is specific nomenclature for abnormal values:
The karyotype is determined by a blood test and allows us to learn the chromosome count and structure. A normal male karyotype is 46XY.
Both the eggs and sperm contain half the chromosomes. An abnormality in a patient’s karyotype increases the risk of producing sperm with an abnormal genetic information. In such cases, embryos are produced with genetic problems resulting in unsuccessful pregnancies, sterility or recurrent miscarriages.
Therefore, it is advisable to perform a karyotype before undergoing an assisted reproduction treatment like In Vitro fertilisation (IVF).
With an abnormal male karyotype, we have two options available: genetic testing of the embryos by preimplantation genetic diagnosis (DGP) before transferring them or using donor sperm.
The genetic testing of sperm is performed in the following cases:
Of the 46 chromosomes that our cells have, 23 come from the father and 23 from the mother. Eggs and sperm have half the chromosomes compared to the rest of the cells. This way, as a result of the union of an egg with a sperm, the embryo has 46 chromosomes. The process that reduces the number of the chromosomes to half is called meiosis. Meiosis only takes place during egg and sperm production.
Occasionally, errors occur during meiosis. These abnormalities imply a worse reproductive prognosis by increasing the amount of abnormal sperm, which does not mean that all of them are necessarily affected. Abnormal meiosis is generally associated with an abnormal semen analysis (especially with oligozoospermia), but it can also be in men with normal semen analysis.
FISH
Sperm normally have 23 chromosomes, even though they may have one extra chromosome or one less, or even have all 46 original chromosomes from the precursor cell. The FISH test examines a certain number of sperm chromosomes. A pathological result indicates that the percentage of abnormal sperm is more than the normal population. The great advantage of this test is that it is easy to perform since it is done directly on the sperm sample.
The limitation of this technique is that only a certain number of the sperm’s 23 chromosomes are examined, which could lead to a normal result for a man who actually has genetic abnormalities. For men with low sperm count, this technique might lead to no result at all due to the lack of material.
Testicular biopsy
The testicular biopsy allows us to directly examine the meiosis process. The procedure is simple and can be performed on an outpatient basis, under local anaesthesia. In this way, the chromosome division can be examined throughout the different phases of meiosis, which makes it much more specific and sensitive for diagnosing abnormalities than a FISH test. This is considered the conclusive test in genetic testing of the male factor.
The DNA carried by the sperm in its head can be damaged by the action of free radicals produced in oxidation reactions. Both primary processes in the testis and external factors affecting the epididymis (the duct in which sperm mature) can cause oxidative stress that damages sperm DNA. A sperm with damaged DNA is more likely to cause embryo quality problems, increasing the risk of implantation failure or miscarriage. Having good quality eggs can reduce this risk as they have a greater capacity for repair.
In general, DNA fragmentation studies are recommended in the following cases:
Using the Comet technique, DNA fragmentation can be examined in a semen sample. The study will tell us whether there is single or double strand damage. Double strand damage always has a worse prognosis, especially when its values are high, and can even cause chromosomal abnormalities in the embryos that increase the risk of miscarriage.

CFTR gene mutations are associated with sterility problems and we find them related to cases of azoospermia and bilateral and unilateral absence of vas deferens.
Given it is a genetic mutation, it can be transmitted to the offspring, also handing down the problems these abnormalities cause. If the same mutation is also handed down by the mother, cystic fibrosis will be triggered.
To avoid problems stemming from this mutation, it is always recommended to investigate the couple carefully and perform preimplantation genetic diagnosis on the embryos during a cycle of In Vitro fertilisation (IVF) in order to transfer healthy embryos.
A varicocele is a venous dilation that drains the testicle. It can be associated with testicular discomfort, although it is not rare enough to be asymptomatic. The varicocele is also associated with an increased risk of DNA fragmentation.
The diagnosis is made by physical examination. A testicular Doppler ultrasound is a useful additional test since it detects abnormal blood flow in the veins, which is associated with the varicocele.
In low level or asymptomatic cases, it is very controversial that its treatment improves fertility. In severe cases, surgery is recommended.