When you are trying to have a child, it is normal for many doubts related to fertility to arise. Understanding the factors involved and knowing the tests that can be performed to improve the chances of success can help reduce anxiety and allow informed decisions to be made. In this new edition of "Fertility Update", we answer some of the most frequently asked questions that arise around fertility.
What does it mean to have a low ovarian reserve?
Ovarian reserve refers to the number of eggs a woman has in her ovaries at any given time. Having a low ovarian reserve means that the number of eggs available is less than expected for your age.
Women are born with a fixed number of oocytes that steadily decreases throughout life. It is estimated that they are born with approximately one million oocytes, reducing to about 400,000 at puberty. Of these, only about 400-500 will be ovulated during the reproductive life.
The main cause of a low ovarian reserve is age, especially after the age of 35. However, other factors can also contribute, such as premature ovarian failure, diseases such as endometriosis or chronic infections, genetic factors, cancer treatments such as chemotherapy, and unhealthy lifestyle habits.
What happens if a woman has low ovarian reserve?
Having a low ovarian reserve does not necessarily mean that the eggs are of poor quality. A young woman can get pregnant naturally even with a low ovarian reserve. However, as the ovarian reserve decreases, the follicles become less sensitive to sex hormones, requiring further stimulation for the egg to mature and ovulate. This lowers the chances of pregnancy.
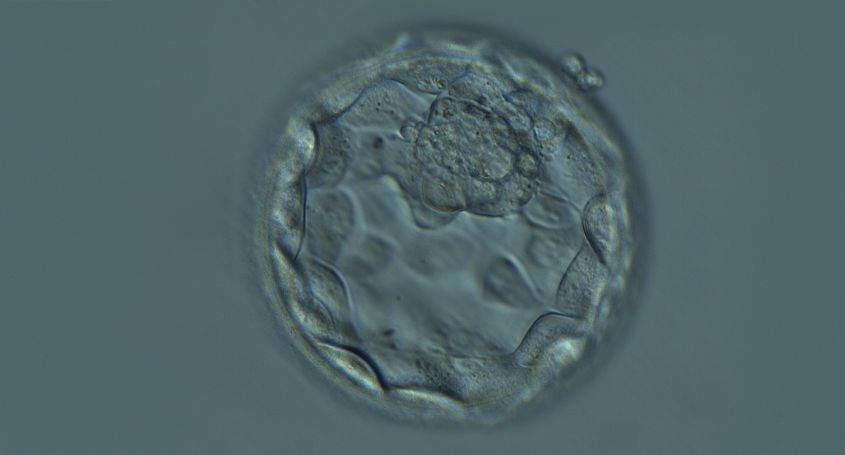
In addition, with age, the quality of the eggs also decreases, so women from the age of 35 may have more difficulty achieving pregnancy naturally. Ovarian reserve is also associated with the number of oocytes that are retrieved after ovarian stimulation. In women with low ovarian reserve, the number of oocytes retrieved will be lower compared to women with a normal ovarian reserve.
As a consequence, it may be necessary to perform several cycles of ovarian stimulation to accumulate enough mature oocytes, thus improving the chances of success in assisted reproduction treatments.
Why do some people get a karyotype before deciding to have children? What diseases are detected in the karyotype?
Karyotyping is a genetic test that looks at the shape, size, and number of chromosomes. In humans, a normal karyotype consists of 23 pairs of chromosomes from each parent, consisting of 22 pairs of autosomes and one pair of sex chromosomes that will be XX in females and XY in males.
Changes in the number of chromosomes are associated with some syndromes, such as Down syndrome in the case of trisomy of chromosome 21, Klinefelter syndrome when chromosome 23 contains an additional X in addition to the Y chromosome (XXY) or Turner syndrome when chromosome 23 is made up of a single X (XO).
Alterations in the structure of chromosomes include deletions, inversions, or translocations. Depending on the size and location of the alterations, they may have no effect, cause health problems or be a cause of infertility.
Couples with reproductive problems have chromosomal abnormalities more frequently than the general population, so the karyotype study is usually a basic test before starting in vitro fertilization treatment. A karyotype is recommended when there are severe sperm abnormalities, ovarian failure, repeated miscarriages and implantation failure s.
What is the genetic compatibility test?
The genetic compatibility test is a DNA sequencing test that analyzes hundreds of genes to identify the presence of possible mutations associated with hereditary diseases and detect if there are any common mutations in both members of the couple.
Some diseases are caused by recessive mutations, meaning that both the maternal and paternal copies of the gene need to have the mutation.
Hereditary genetic diseases can be prevented thanks to the genetic compatibility test, as it allows to determine if the members of the couple are carriers of these diseases.
It is usually performed before assisted reproduction treatment, before treatment with an egg or sperm donor , in couples with a history of a genetic disease or in consanguineous couples.
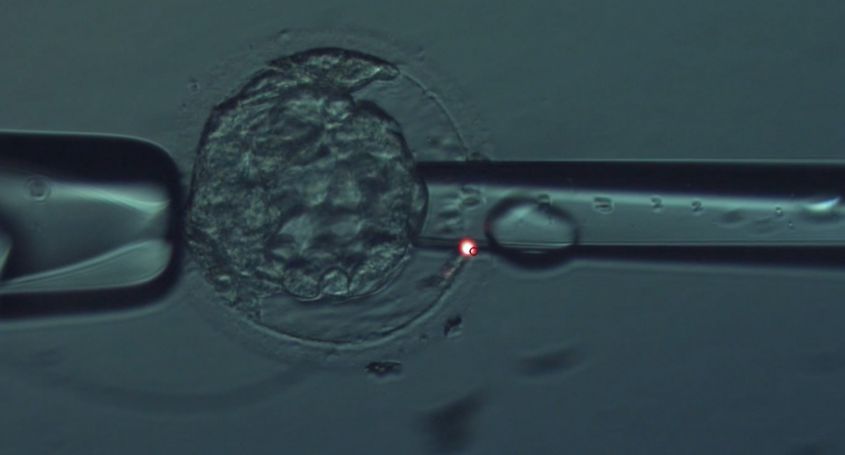
If it is detected that both members of the couple are carriers of a mutation in the same gene, it is advisable to carry out an in vitro fertilization treatment with preimplantation genetic diagnosis to select those embryos not affected by the mutation of the gene to transfer them to the uterus. Another option to avoid the transmission of the genetic disease is to opt for gamete donation.