In Vitro fertilisation Spain

What are the steps of the process?
In Vitro fertilisation (IVF) consists of 3 main steps:

In Vitro fertilisation and embryo culture

How is the treatment performed?
Find out everything you need to know.
General information
In Vitro fertilisation (IVF) is recommended in the following cases:
- Obstruction of the fallopian tubes
- Male factor that cannot be resolved with artificial insemination
- Low ovarian reserve
- Genetic diseases that require preimplantation evaluation
- Aged 38 or over
- Previous insemination failure
- Long-term sterility
To perform In Vitro fertilisation (IVF), previous examination with the following diagnostic tests is necessary:
- Hormone test to examine the ovarian reserve. The Anti-Müllerian Hormone (AMH) value can be determined at any time during the cycle, and the FSH and Estradiol value on day 3 of the cycle.
- Semen analysis to evaluate the quality of the sample. If sperm quality is very low, it will be necessary to extend the andrological examination with other additional tests.
- Gynaecological ultrasound to rule out uterine and ovarian diseases. It is also used to evaluate the ovarian reserve by antral follicle count.
- Karyotypes to rule out genetic abnormalities which may affect the embryo.
- Serologic test to dismiss the presence of transmissible infectious diseases.
Ideally you should wait until the ovaries return to their normal condition before stimulating them again for In Vitro fertilisation. It is recommended to wait a couple of cycles before performing another treatment.
There is no limit to the number of in Vitro fertilisations (IVF) but it is usually not more than 3. It is convenient to re-evaluate the case after each cycle which did not achieve a pregnancy, in order to determine whether more tests are necessary
The most important risks of In Vitro fertilisation (IVF) originates from:
Ovarian stimulation:
Hyperstimulation syndrome may occur due to the excessive response of the ovaries to the medication. This risk is currently minimal since individualised protocols are performed.
Ovarian puncture:
Bleeding can occur, which is generally self-limited. In rare occasions surgery will be required to solve this.
Multiple pregnancy
The single embryo transfer policy is helping to considerably reduce considerably the number of multiple pregnancies.
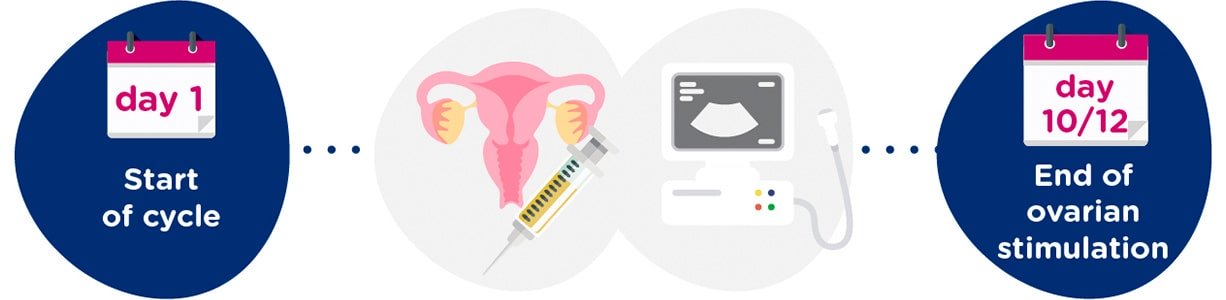
Ovarian stimulation and gynaecological tests
In certain cases, such as in women with low ovarian reserve or those who need to maximise the number of oocytes in a short period of time, the DuoStim technique can be used. This technique consists of performing two consecutive ovarian stimulations within the same menstrual cycle: the first during the follicular phase (beginning of the cycle) and the second in the luteal phase (after ovulation). In this way, it is possible to obtain egg cells at two different times during the same cycle, optimising the total number of retrieved oocytes without having to wait for the next cycle.

Egg and sperm collection, fertilisation
The sperm used for In Vitro fertilisation can come from the partner’s sperm sample or donor sperm.
In the event of using donor sperm, it will be chosen as set out by Law, maintaining the maximum phenotypic similarity with the patients.
The most common way of collecting sperm is through masturbation on the day of egg collection. Where necessary, a previously frozen sperm sample can be used.
Other ways of collecting sperm are testicular aspiration (TESA) and testicular biopsy (TESE). Both techniques are used when no spermatozoa are found in the ejaculate.
In case donor sperm is used, the sample will always be frozen.
Fertilisation is performed in the laboratory after egg collection. The laboratory techniques for inseminating eggs are conventional IVF, intracytoplasmic sperm injection (ICSI) or intracytoplasmic morphologically selected sperm injection (IMSI).
ICSI is currently the most common technique of choice to inseminate eggs in the majority of cases, especially if there has been a history of fertilisation failure or very poor sperm quality.
We recommend using IMSI when there is severe teratospermia or high sperm DNA fragmentation.
For the remaining cases, if we have a good number of mature eggs, conventional IVF can be used.
18-21 hours after inseminating the eggs, its correct fertilisation is checked. The embryos will remain inside an incubator, which provides the ideal conditions for their development. These incubators can be conventional or with time-lapse technology.
The progress of each embryo will be examined every day until day 5 of development when its transfer inside the uterus will take place. This long culture of 5 days allows us to select those embryos (blastocysts) with the best implantation capacity, thereby increasing the chances for a pregnancy.
Embryo transfer
If there are still some good quality embryos after embryo transfer, they will be frozen.
The transfer of frozen embryos just requires good endometrial development by the woman. Therefore, an oral or transdermal hormone therapy is used which is administered from the start of the cycle. A few days later, we check that the endometrium has been prepared correctly and the transfer day is arranged.
The embryos are thawed on the day of their transfer. If the frozen embryos are of good quality and, even more if they are blastocysts, their survival rate is higher than 90%.
The embryos can stay frozen until their final destination established by law. is decided. The freezing time does not affect the results.

Positive results
In Vitro fertilisation (IVF) is one of the best assisted reproduction treatments available. Its success rates depend mainly on the woman’s age, with the cumulative rate of pregnancy per cycle of more than 50% until the age of 39 and gradually decreasing from then on.
Women aged < 35
Aged between 18 and 35
Aged between 39 and 42
Women aged < 42
What does in vitro fertilization treatment include?
In vitro fertilization treatment includes:
- Medical appointments
- Follicular puncture
- Transfer
- Ultrasound scans during the cycle
- ICSI
- B-hCG
- Hormone tests
- Embryo culture